Is non-operative management of childhood neurologic cavovarus foot effective?
Introduction
요족에 대한 치료는 서로 다른 많은 의견들이 충돌한다. 요족의 자연적 진행은 아동의 성장과 요족을 진행시키는 신경학적 병인으로 인하여 좋지 않은 결과를 초래하는 경우가 많다. 요족으로 인한 변형은 다음과 같은 기능적인 증상을 유발하는데, 발목과 발바닥의 통증과 5번째 중족골의 기저부분과 첫번째 중족골의 골두에 굳은살이 잘 생긴다.
변형이 더 진행되면 전족부의 회내 혹은 외반과 후족부의 회외 혹은 내반이 일어나서 종족부 단위(calcaneopedal unit)의 비틀림이 유발된다. 전통적인 요족의 병인은 전경골근과 단비골근의 기능이상이며 이차적으로 내재근(intrinsic muscle)의 기능저하이다. 이에 대한 대표적인 질병은 샤코-마리에-투스 (Charcot-Marie-Tooth disease)로 알려져 있다.
요족의 진행과정에서 내재근의 위약으로 인한 중족지관절의 불안정화가 발생하고 길항근인 장족지신근과 장무지신근은 활성되어 중족지관절의 과신전을 유발한다. 이는 첫번째 발가락의 족저건막(plantar aponeurosis)의 장력을 증가시켜 족저궁(plantar arch)의 높이를 증가시킨다.
요족의 진행과정에서 후족부의 변형은 초기에는 유연한 내반 변형을 나타내지만 성장에 따라 점차로 굳어진다. 요족의 환원성에 대한 검사는 전족부의 영향을 배제하고 거골내반을 교정해 보는 Coleman and Chesnut’s block 검사가 있다. 정리하면 요족(cavovarus)는 전족부의 변형이 먼저 일어나고 이에 따라 후족부가 변형되는 것이다.
그러므로 우리는 비수술적인 치료가 유년기에 요족의 교정을 충분히 할 수 있다는 가정하에 Untwisting nocturnal splint 와 Untwisting walking cast 를 개발하여 적용해 보았으며, 세부적으로 Splint 이전에 Cast 를 적용하는 것이 치료에 더 효과적일 것이라고 생각하였다.
Material and Method
2002년부터 2010년까지 8년동안 23명, 35족을 대상으로 연구를 진행하였다. 요족의 원인은 샤코-마리에-투스(15명,22족), 뇌연화증(3명,5족), 뇌성마비(2명, 3족), 척수열개(1명, 1족), 염색체이상(1명,2족)이었다. 치료를 시작할 때 평균 나이는 8.8세(5-15세) 였으며, 치료 시작 당시 후족부 고정상태에서 체중지지 측면 족부 X-ray 와 Meary angle(거골-제1중족골의 각도) 도 함께 측정하였으며 평균 16도였다. 치료 방법은 3주간 첫번째 Cast 를 적용 후 교정을 위해 두번째 Cast 를 다시 제작하여 3주간 적용하고, 이후 Splint 를 적용하는 순서로 진행한 군이 13족(37)이었으며, 소아의 부모가 cast 를 거부 하여 Splint 만 적용한 군이 22족(63%) 이었다. Splint 는 성장 종료시까지 적용하였다. 치료 종료 시점에서 Wicart-Seringe Grades(Table 3)를 적용하여 결과를 비교하고, Mann-Whitney test 로 분석하였다. 경과가 좋지 않아 수술을 한 경우는 모두 Poor Grade 로 분류하였다.
Untwisting walkinig cast (Table1, Fig.1.)
|
Deformity |
Action by surgeon |
Action by assistant |

|
|
Cavus and equines
Adduction of
calcaneopedal unit
Talar varus
Forefoot pronation |
Ankle at 90◦
Lateral rotation (abduction) of foot
Mediolateral pressure on heel
Forefoot supination,
Maintaining mediolateral pressure on heel |
Pressure on knee
Medial rotation of leg
Lateromedial pressure on leg
No specitic action |
Untwisting nocturnal splint (Table2, Fig.2.)
|
Effect of splint |
Deformity component coreected |

|
|
Ankle at 90◦
Forefoot supination
Hindfoot valgus
Dorsolateral strap |
Cavus and equines
Forefoot pronation
Hindfoot varus
Cavus, dorsal hump and hindfoot varus |
Table 3. Wicart-Seringe grades
|
Results |
Functional signs |
Clinical position of heel and Méary angle |
|
Very good |
None |
VG, and 0◦ ≤ Méary angle ≤ 15◦ Or N or VR, and 0◦ ≤ Méary angle ≤ 5◦ |
|
Good |
None |
VG, and 15◦ < Méary angle ≤ 20◦ Or N, and 5◦ < Méary angle ≤ 20◦ Or VR, and 5◦ < Méary angle ≤ 15◦ Or −15 ≤ Méary angle < 0 (minor hypercorrection) |
|
Moderate |
None |
VG or N, and Méary angle > 20◦ Or VR, and Méary angle > 15◦ Or Méary angle < −15◦ (major hypercorrection) |
|
Poor |
Pain and/or instability |
VR, and Méary angle > 20◦ Or cavus surgery |
VG: talar valgus; N: heel in neutral position; VR: talar varus
Result (Table4)
임상적으로 65%에서 Very Good 또는 Good Grade 를 보였고, 기능적으로 79% 에서 호전되었다.
후족부 내반은 25족(69%) 에서 교정되었다. Meary Angle 은 치료적 평균 16도에서 치료 종료 후
평균 7.5도로 감소하였다. 그림 3과 4는 임상적, 방사선적으로 좋은 결과의 예를 보여준다
Table 4 Results according to Wicart-Seringe grade
CMT: Charcot-Marie-Tooth disease; C + S: casts + splint; S: splint.
|
|
Whole series
(n = 35) (%) |
CMT
(n = 22) (%) |
Other etiologies
(n = 13) (%) |
C + S
(n = 13) (%) |
S
(n = 22) (%) |
|
Very good result
Good result
Moderate result
Poor result |
15(42)
8(23)
1(3)
11(32) |
11(50)
5(23)
1(4)
5(23) |
5(38)
2(16)
1(8)
5(38) |
7(54)
4(31)
2(15) |
8(36)
1(5)
3(14)
10(45) |
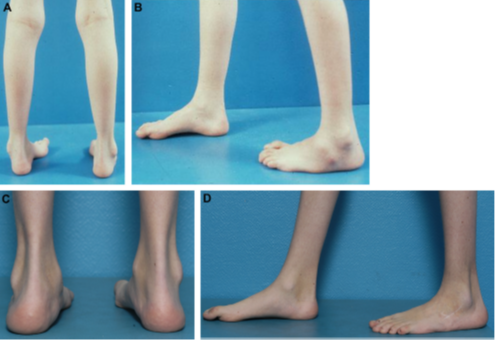
Fig. 3. Clinical result in a 10-year-old girl with Charcot-Marie-Tooth disease. A and B. Initial aspect of foot: indication for surgical correction (POWOC) in left foot (moresevere) and cast + splint in right foot. C and D. Result at 16 years: very good
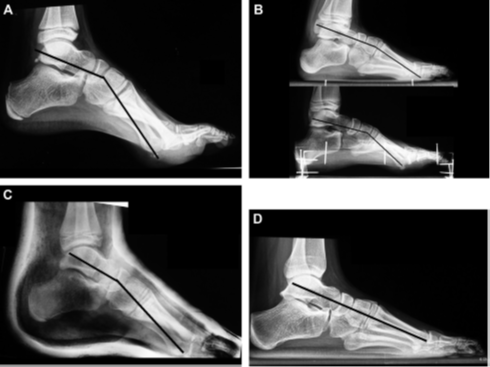
Fig. 4. Radiologic result in an 11-year-old girl with Charcot-Marie-Tooth disease. A. Pre-treatment weight-bearing radiograph: maximal cavus (Méary angle = 33◦). B. Pre-treatment weight-bearing radiograph: above (without block): Méary angle underestimated (15◦); below (with block): true Méary angle of 29◦. Cavus lessened in weight-bearing. Transverse defects not completely reducible. C. Untwisting walking cast: incomplete correction of cavus (Méary angle = 17◦) but complete correction of transversedefects. D. Result at 18 years: complete correction of cavus and transverse defects.
Discussion
이 연구의 제한점은 피험자 수가 적고, 비진행성 및 진행성 족부를 모두 포함하고 있으며, 치료 시작 전에 요족의 정도를 평가하지 않았다는 것이다.
그동안 비수술적 요족의 치료를 시행한 한 건의 연구에서는 좋지 않은 결과를 보고 하였으나, 6주만 Splint 를 착용하였고 성인을 대상으로 하여 골의 재형성 기회가 없었다는 점에서 이 연구과는 차이가 있다. 본 연구에서 시행한 교정은 효과적이었으며, 수술의 위험성을 감소시켰다. 또한 수술이 필요한 경우에도 평균 4.5년을 연장시켜 단일 단계의 교정이 가능하며, 반복수술을 하지 않고 수술 후의 잔여 성장에서 발생할 수 있는 변형을 예방할 수 있는 것으로 여기진다. 또한 Splint 만 하는 것보다 Cast 이후 Splint 를 적용하는 것이 수술의 위험성을 감소시키지는 않지만 적어도 Meary Angle 교정면에서는 더 효과적임을 확인하였다.
치료 시작 당시 10세 미만의 어린 나이에서는 예후가 좋지 않았다. 이러한 이유는 변형의 진행과 성장이 끝나기 전 재발이 있었기 때문이었다. 또한 Splinting에 대한 불량한 순응도도 좋지 않은 예후 인자였다. 이 연구에서 Cast 와 Splint 를 연속으로 적용하는 것에 대한 합병증은 없었지만 샤코-마리에-투스 병과 같은 민감한 질병의 환자에게 캐스트와 부목을 적용할 때에는 주의를 기울이는 것이 바람직할 것으로 생각된다.
Conclusion
이번 연구는 소아에서 신경인성 요족의 비수술적 치료의 효용성을 입증하였으며 수술을 피하거나(성장 말기 50%에서) 평균 4.5년을 연기하였다. Meary Angle 이 15도가 되면 바로 Untwisting walking cast 이후 Untwisting nocturnal splint 를 적용하는 것을 권장한다.







